Streamline call center operations with automation

Photo: sturti/Getty Images
Healthcare call centers perform vital functions such as connecting patients to caregivers and managing scheduling, billing, and triage requests. Despite playing such a crucial role, the call center is often neglected and underserved when it comes to technology. Even after the adoption of the electronic health record (EHR), most healthcare call centers are still the primary way patients access care, even though most patients do not want to use the phone for such tasks. Call center automation can drive efficiencies by reducing call volume and enabling patients to engage with providers via their preferred channels.
Automation enables patients to self-schedule appointments and fill out intake and registration forms when and where it's most convenient for them, giving patients more control over their care experience. Implementing automated, digital-first experiences means health systems can rely less on their call centers. If you’re ready to reduce your organization’s reliance on its call center, three proven steps can help get you there.
Step 1: Identify the workflows with the highest potential for return on investment (ROI)
Research indicates that most patients do not want to schedule care via phone. However, more than 70% of call center volume comes from appointment scheduling, rescheduling and cancellations.
Perform an analysis of current inbound and outbound call volumes. Use this as a baseline and segment different categories for high-volume calls. Using this trend data, calculate the total time spent on each call type to use as a general proxy for potential automation ROI.
With this initial data, assess what percentage of your current call volume could be automated. For example, can inbound calls to your call center be redirected to a self-service tool? Along with this analysis, assess the following factors that contribute to the overall value of managing a call with automation as opposed to staff:
● Complexity: How easy or difficult is training agents to perform the task effectively? Can the task be broken down into repeatable, standardized steps? Manual patient verification may require staff to access multiple systems and demands delicate handling to comply with privacy rules, while automation technology can quickly and accurately verify patients through voice recognition.
● Patient impact: How much value does a human touchpoint add or subtract from the interaction? Patients may not see much difference in getting an appointment reminder via call or voicemail compared to an automated text, but they may prefer to speak to a human regarding payment reminders for a large outstanding balance.
● Cost of an error: How much value is lost when agents make mistakes? Consider how, for example, front-end registration errors can lead to back-end denials that are expensive to address.
● Difference in performance: How much more or less effectively can the workflow be performed by a person? Artificial intelligence (AI) tools can be more accurate than trained staff in selecting the correct insurance plan for billing.
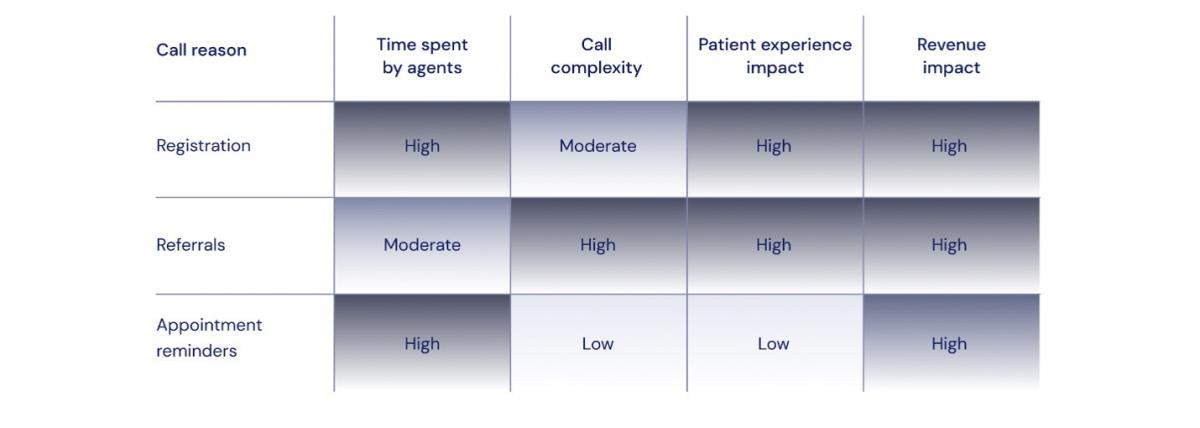
The following table identifies three workflows that health systems generally start with to establish effective contact center automation.
Step 2: Find the right automation partner and create an implementation plan
When it comes to healthcare automation and AI technology, choosing the right partner is critical. The ideal call center automation partner will collaborate seamlessly with your IT department. They will work closely with your implementation team to consider all perspectives, and they will not take a transactional approach to call center automation. Instead, the focus will be on building a long-term relationship based on mutual growth and success.
The following are five areas of emphasis that can help ensure a smooth implementation.
● Project planning: A detailed project plan should include key tasks, timelines, and responsibilities. This will be the guide that helps set expectations and keep the project on track.
● Technical assessment: Thoroughly review existing infrastructure and identify any technical constraints that must be addressed before implementation.
● Data migration: Healthcare call centers frequently handle highly sensitive data like patient records and billing information. It is essential, and sometimes even regulated, that moving data between systems be completed without loss or corruption. Apply a rigorous data mapping process to determine how data from the old system will fit into the new one.
● Integration with existing systems: Your chosen call center automation platform must work seamlessly with your EHR. Don’t overlook other critical tools, such as customer relationship management (CRM) software, since protected health information (PHI) must flow securely between systems to maintain compliance.
● Equal attention to patient and staff experiences: Automations that make things easier for the patient but still require manual administrative work for staff only solve half of the problem.
Modern health systems need technologies that deliver a highly personalized patient experience on the front end while eliminating back-end administrative work.
Step 3: Measure the impact and iterate on your call center automation over time
Even the best-planned call center automation program can improve after implementation. The most successful health systems embrace an iterative approach, which means focusing on the highest-priority workflows that will drive the most value first.
Once priority automations are in place, gather feedback from patients and staff. Surveys and focus groups can help identify problems with the technology or training. Any identified issues should take precedence in terms of handling. Collecting baseline data like call duration, first call resolution rates and agent idle times also helps leadership determine the effectiveness and efficiency of implemented automation.
Here are several key performance indicators (KPIs) to consider in evaluating call center automation:
● Patient satisfaction
● Average handle time (AHT)
● Call volume
● Call deflection rates
● Agent or staff time saved
Transforming patient access through call center automation is not just a technological upgrade, but a strategic initiative that redefines the patient experience and operational efficiency. By identifying high-ROI workflows, partnering with the right automation experts and adopting an iterative approach to refinement, healthcare organizations can shift from a reactive to a proactive model of care.
This reduces the burdens on call centers and allows agents to focus on the most complex patient challenges to help better drive patient loyalty. Automation also empowers patients with the convenience and control they desire, ultimately leading to improved satisfaction, reduced costs and enhanced access to care. Embracing these three essential steps can turn healthcare call centers from bottlenecks into breakthroughs.


























