Working towards a Clinically Integrated Healthcare Supply Chain with H-SIMM
At HIMSS18, HIMSS Analytics and SCAN Health announced its collaboration on the Health-Supply Information Maturity Management (H-SIMM), a supply chain maturity model to help organisations advance their digital maturity in supply chain infrastructure.
As part of this collaboration, SCAN Health designed and created the health supply chain maturity tool while HIMSS, with its global network of 73,000 partners, is helping build awareness and knowledge.
This November, Dr. Anne Snowdon, Developer of the H-SIMM, Academic Chair of the World Health Innovation Network (WIN) and Scientific Director and CEO of SCAN Health, is speaking at HIMSS AsiaPac18 in Brisbane, Australia.
Dr. Snowdon is a clinician-turned-innovator. Her early career as an emergency department nurse brought her into contact with many children entering the ER with serious car accident injuries, motivating her to partner with the automobile industry to devise a more effective booster seat. Since then, she has combined her sharp clinical eye with innovation to foresee and resolve challenges across the healthcare system.
Ahead of the November conference, Dr. Snowdon gives us a preview of the H-SIMM model and shares how supply chain is critical to patient care.
What can you share about the H-SIMM model with us?
The H-SIMM model is designed to provide health organisations with a strategic "road map" to guide the integration of supply chain infrastructure (i.e., tools, technologies, processes) into clinical care environments to support quality and safety of patient care and at the system level it strengthens performance of health systems. The H-SIMM is often described as a clinically integrated supply chain strategy - the challenge is that this has many different meanings for different stakeholders in health systems. I define clinically integrated supply chain as an organisational strategy, whereby leaders (i.e., CEO and executive team) view supply chain as a strategic asset that is leveraged to strengthen the performance of the organization - specifically to improve quality and safety while at the same time reducing cost.
This organisational strategy introduces supply chain tools and technologies (ex. inventory management software, point of care scanning or RFID) into care delivery processes to capture product data, care process information and patient and provider data, all uploaded into patient health records to enable automated tracking and traceability of care linked to patient outcomes. This integrated system then creates what I refer to as "real world evidence" of the care processes and use of products (ex. implants, medications) that offer the best outcomes for specific patient populations.
Supply chain staff become fully integrated into clinical program teams whereby the supply chain staff are an integral part of the clinical team working to advance quality, safety and value in every program across the organization. When such a system is scaled across health systems, it creates a robust flow of data in near "real time" to inform system leadership decisions on delivery of programs and care processes that offer the best outcomes for the population the health system is mandated to serve.
What are the outcomes of clinically integrated supply chain?
Automated tracking and traceability of every patient, care process, products used in care linked to outcomes which creates a transparent, powerful data resource to support leadership decisions on how best to strengthen organizational performance.
Evidence emerging from health systems already implementing a clinically integrated supply chain include the following:
a) Safety: Significant reduction (70% reduction reported by Mercy, U.S.) in serious, harmful adverse events often called "never events" - errors that should never happen in healthcare (ex. surgery on the wrong patient, leaving a product in a surgical wound).
b) Quality: Variation in care is widely viewed as a challenge for health systems as some patients receive different care than others, with limited ability to standardize to ensure only best practices are delivered in patient care settings. The traceability of every care process, procedure and product delivered by clinician teams enables leaders to track care being delivered and link it to outcomes to inform clinician teams using objective data what practices are achieving the best results for patients. Evidence to date has identified significant change in clinical practices that offer greater standardization and use of best practices to support quality of care.
c) Value: Health organisations struggle to manage growing costs of supplies, high cost products (ex. implants) and labour costs to sustain a workforce of highly specialized health professionals. Integrated supply chain infrastructure automates care processes which reduces burden on clinician teams and has resulted in reduction of labour costs by 16 FTE's in perioperative programs (ex. NHS, UK). Costs are also reduced as much as 30% per case due to reduced waste of products (ex. Mercy, U.S.) when products are expired and must be thrown out.
What is the current state of digitisation in healthcare supply chains in U.S. and Canada? We’d like to hear about the findings from your qualitative research.
I have not specifically studied digitisation in health systems. However, the key challenges identified by many health systems includes multiple IT systems across organisations that do not connect or interface with each other. The challenge this presents is that a patient's journey of care is never captured in a way that all care providers or clinician teams can identify what care has been delivered, what products (ex. medications) have been prescribed or used and what outcomes have been achieved. Thus, there is no record of the patient's care journey to date.
For example, the primary care physician or team uses a patient record that does not interface with a hospital EMR, hence the hospital teams cannot identify key patient needs and no access to patient information that is needed to inform care decisions. Adverse events occur often during transitions in care when patients receive care from one team (i.e., primary care) and then transition to another team (i.e., hospital team). Digitisation needs to connect care across a patient's journey to advance quality and safety across health systems. The integrated supply chain infrastructure addresses this system level challenge by enabling tracking and traceability across the patient's journey of care to reduce the risk of error, to identify what care is associated with the best outcomes and under what conditions best outcomes are achieved.
In your research at WIN, you are creating empirical evidence of the impact and value of supply chain maturity in health systems. What have you found out?
I would like to share the outcomes for three global health systems: Alberta, Canada; NHS, UK and Mercy, U.S. below. You can view the entire slide deck here.
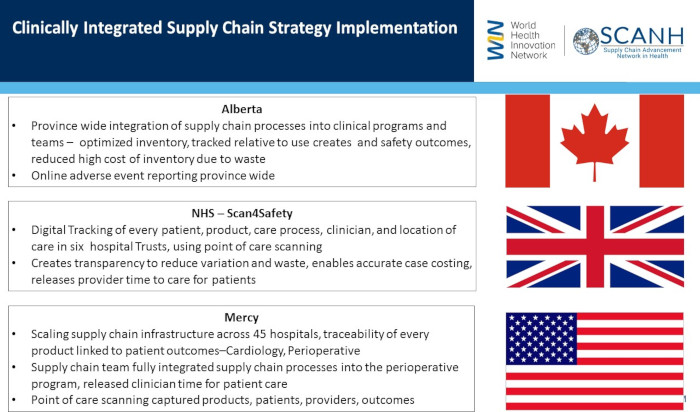
SCAN Health has become a key opportunity for knowledge mobilisation to disseminate these outcomes so that global health systems can learn from each other, avoid duplicating lessons others have already learned and to accelerate progress globally.
Supply chain transformation is both internal and external. Can you share about these internal and external factors and how to achieve success?
Internal: There are two key factors internally that advance supply chain transformation. First is the senior leadership of health organisations who must create the vision and strategy to mobilize teams to advance integrated supply chain infrastructure across the organisation - hospitals or community care settings. Leadership is the single most critical factor that either drives the supply chain strategy or almost always ensures no progress is made if leadership is not driving the initiatives and strategy. The second key factor is clinician leadership. Clinicians so often have little or no line of sight in to what supply chain is and what it can achieve.
Our research has demonstrated that not only engaging clinicians in the strategy, but also creating the conditions for successful clinician leadership is a second internal key condition for success. Clinicians and especially physicians play a pivotal role in supporting the changes in clinical workflow that is needed and championing the use of supply chain data to inform decisions on quality, safety and standardisation of care processes that offer the best outcomes for patients. Physicians are in a unique leadership position to mobilize clinician teams, evidence from both Mercy and the NHS demonstrate clinician leadership as foundational to successful integration of supply chain tools, mobilizing data to create real world evidence that then supports and informs quality and safety initiatives for patients.
External: The role of policy is critical for creating the momentum for health systems to implement supply chain infrastructure across the many organizations. When legislation requires adoption of global standards, both industry and health organisations are incentivised to implement supply chain infrastructure. For example, the FDA in the U.S. has now required use of global standards on products such as implants to enable traceability and reporting outcomes. The EU legislation similarly requires use of global standards and automated e-commerce which has now motivated automation of these key processes.
These policy frameworks are critically important in building awareness, knowledge and creating the incentives to implement integrated supply chain infrastructure. The second external factor that is a key factor for success is establishing a collaborative model that brings all the key stakeholders together to mobilise their respective expertise and leadership to create momentum and accelerate progress.
The collaboration model at both WIN and SCAN Health engages industry, government, academia and health sector leaders, which when all working towards a common goal, can support success. Each of these key stakeholders are critical to the system vision and perspective and policy must be framed to support and drive progress. Health system leaders need to drive the strategy and mobilise resources, clinician leaders need to bring their expertise to ensure supply chain tools strengthen work environments and meet patient care needs and industry must bring their tremendous supply chain expertise to the collaboration to support and ensure global traceability across borders is achieved at the system level. This collaborative model considers those internal and external factors to achieve successful adoption.
About SCAN Health
SCAN Health is an international knowledge translation platform funded by the Government of Canada, Networks of Centres of Excellence (NCE) and hosted by the University of Windsor’s Odette School of Business. Spanning five countries, including Australia, the Netherlands, the United Kingdom, the United States and Canada – and with over one hundred partners from industry, healthcare, government and academia – SCAN Health will advance global capacity to adopt and scale best practices in healthcare supply chain to offer traceability of products and care processes from bench to bedside to patient outcomes.
About WIN
The World Health Innovation Network is based at the Odette School of Business at the University of Windsor, under the leadership of world renowned researcher Dr. Anne Snowdon. WIN brokers partnerships between key stakeholders to source, embed and scale innovations in health systems. WIN develops the evidence of impact and scalability across health systems and disseminates this information to accelerate health system transformation, drive economic growth and improve patient outcomes.
Dr. Anne Snowdon is a speaker at HIMSS AsiaPac 18 in Brisbane this November. To learn more about this event, click here.





















