Health IT interoperability by example

Health IT interoperability is hard. But is it really as hard as it is being made out to be?
ONC has a ten year roadmap to its achievement…but a recent survey says providers don't believe that even ten years will be enough if we stay on the current course. Congress is threatening legislation about EHR "data blocking"…but it is not clear that data blocking is a real obstacle to interoperability. Some are saying that "the industry" should now lead... but there were many unsuccessful years of that. The federal health IT advisory committees are convening yet again to ask what it will take to get to interoperability… but there is no reason to think that the outcome will be different this time. The "once-in-a-lifetime" HITECH incentive program is all but finished…but now, the National Coordinator, Karen DeSalvo, has said that more should have been done to advance interoperability from the start.
And yet, with all the confusion and the limited progress of general health IT interoperability, electronic prescribing (eRx) has moved smartly from concept to operations over a similar time period. There are certainly differences and caveats related to using eRx as an example for the broader activity. And many prescriptions are still not executed electronically – but interoperability is not the reason. And there are some clear lessons to learn here.
Part of the interoperability problem is it means a lot of different things to different people. In its most complex and abstract form, interoperability and particularly "semantic interoperability" can involve complex medical concept representation issues or highly technical medical device connections. But for many people interoperability means general information exchange – like sharing a prescription electronically between a provider and a pharmacy – as the majority focus of what practical interoperability needs to be. Yes, even in eRx, complex knowledge representation is needed for really helpful decision support, but you can get the process "going" with simpler considerations. And if the process is not "going" you can't get to the decision support anyway.
[See also: Where's the plan for interoperability?]
The health IT interoperability area is so confused now that we really need to look to some very practical examples of where interoperability has been solved, at least at an entry-level, and stop some of the hand-wringing, angst, and casting about. The federal government moving into the next administration and the post – Meaningful Use era, particularly needs to focus its attention and programs to develop "entry-level" interoperability to justify the public's 30 billion dollar EHR investment and make EHR data serve broader health outcomes for patients and populations.
Interoperability by example
The following table identifies several areas involved in interoperability. It lists some attributes of the general health IT interoperability situation for each area and does the same for electronic prescribing. And then it draws some select lessons from the comparison.

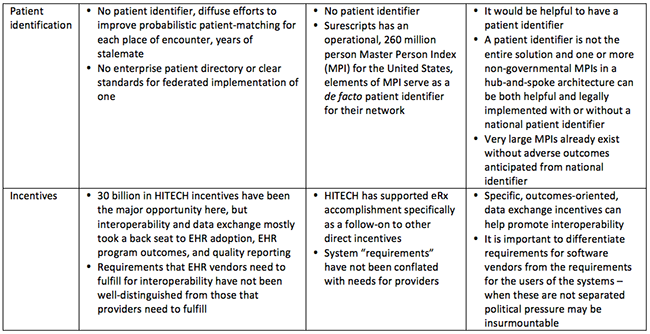
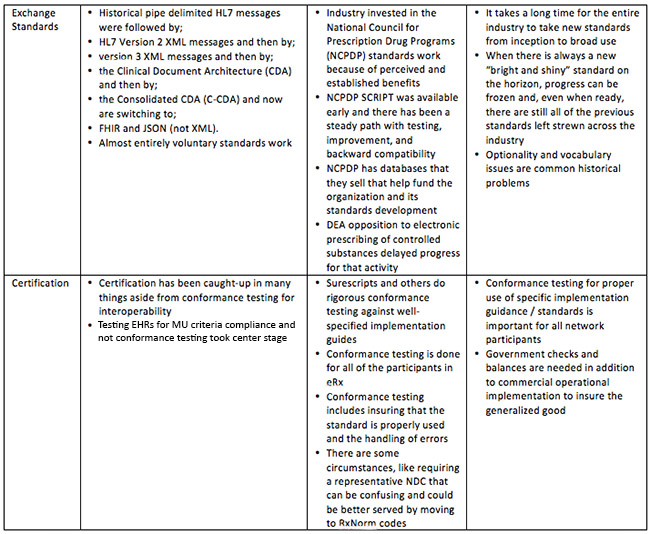
General health IT and eRx are not exactly the same, but there are relevant lessons to learn by comparison. Even some of the differences, like the specificity of eRx vs. the diffuse nature of "general health IT," is important fodder for consideration. There is now a lot of discussion of needing to closely track "business outcomes" to focus interoperability work and eRx is a useful example of this.
There are also several high-level lessons that seem evident from the comparison to eRx:
1. Initial health information exchange the supporting transactions for all participants are an important pre-requisite and priority. More complex concept representation, terminology adherence, and services are important, but are not foundationally critical.
2. Functional "networks" are an important component of moving data. An often shifting and now laisez-faire networking approach has not worked for general interoperability and has left us with no clear networking path forward.
3. Consistency and persistence in approach are important. One benefit of having commercially – leaning network operations is that those who are managing a network on a day-to-day basis know how hard it is to change course. They push back against the otherwise strong tendency to always be chasing the next "bright and shiny" standard, technology, or approach. Sure, it all gets better, but interoperability could have been achieved with each level if we were focused enough.
[See also: Interoperability: for real this time?]
Terminology standards and knowledge representation are not more advanced in the eRx domain and some eRx outcomes, like more sophisticated decision support, still will have to await further semantic specification. But the operational network and organizational interoperability elements are much more clearly developed.
More attention to how networks are technically and organizationally constructed has moved eRx into operations faster and shown that interoperability is substantially achievable in less than ten years. Achieving interoperability for the broader health IT world will require a laser-like focus and persistence that is not easy to find as federal administrations change. One important tool will be to consider what is already working elsewhere.
The author would like to thank Tom Bizzaro, R.Ph of FDB (First Databank Inc.) for his contributions and comments.

























